Round out your Mammography QA program with proven tools, including Breast Compression QC Device, High Purity Aluminum HVL Set, Aluminum Step Wedge, and Phototimer Consistency Tools.

Mammo Digital Compression Device
Measure compression force to assure accuracy and reproducibility.
- Removable display panel supports prone and standard mammo systems, with compression force up to 34 kg (Mammo Digital Compression Scale)
- Backlit LCD screen displays force in standard or metric units, with continuous monitoring for time study (Mammo Digital Compression Scale)
- Foam-lined tray and foam compression block support and protect curved paddles (Mammo Digital Compression Scale)
- Analog readout easily legible from multiple viewpoints, maximum force reading memory, and 1-button reset (Breast Compression QC Device)

High Purity Aluminum HVL Set
Measure half value layer in support of MQSA requirements.
- Ultra-thin and ultra-high purity 99.99% aluminum sheets
- Includes 6 sheets and storage case

Aluminum Step Wedge
Examine the effects of changing the digital image receptor settings and film-screen combinations
- Economical and easy to use
- Made of high purity aluminum, with 9 steps ranging in thickness from 0.3 mm to 2.27 mm

Phototimer Consistency Tools
Test Automatic Exposure Control (AEC) performance.
- Economical and easy to use
- Includes 7 pieces
- Choose either acrylic or breast tissue equivalent (BR) material
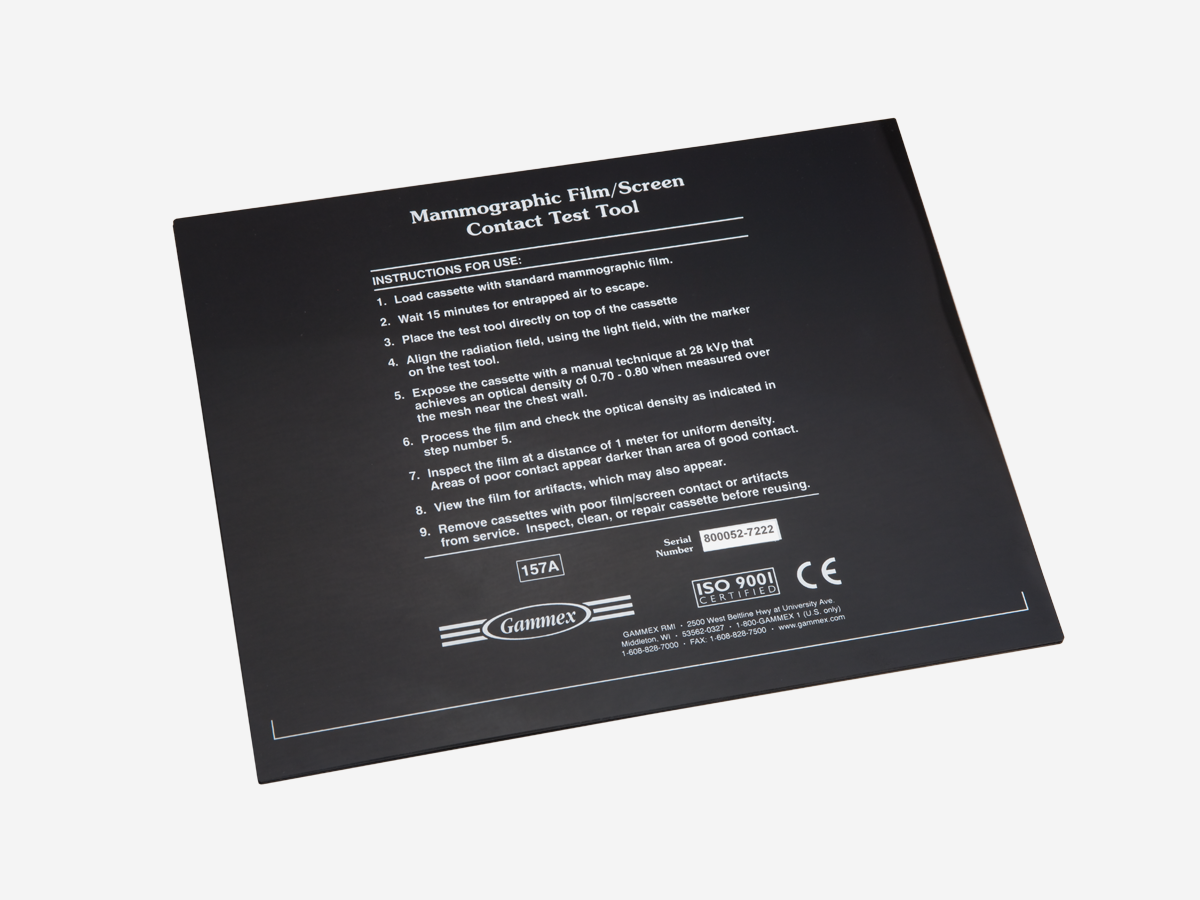
Mammo Film Screen Contact Test Tool & DCF Test Tool
- Supports early artifact detection in screen film systems (Mammo Screen Contact Test Tool)
- Records up to 11 exposures on one piece of film for quick, accurate assessment of a film-screen mammography unit’s Automatic Exposure Control (AEC) accuracy (Density Control Function [DCF] Test Tool)

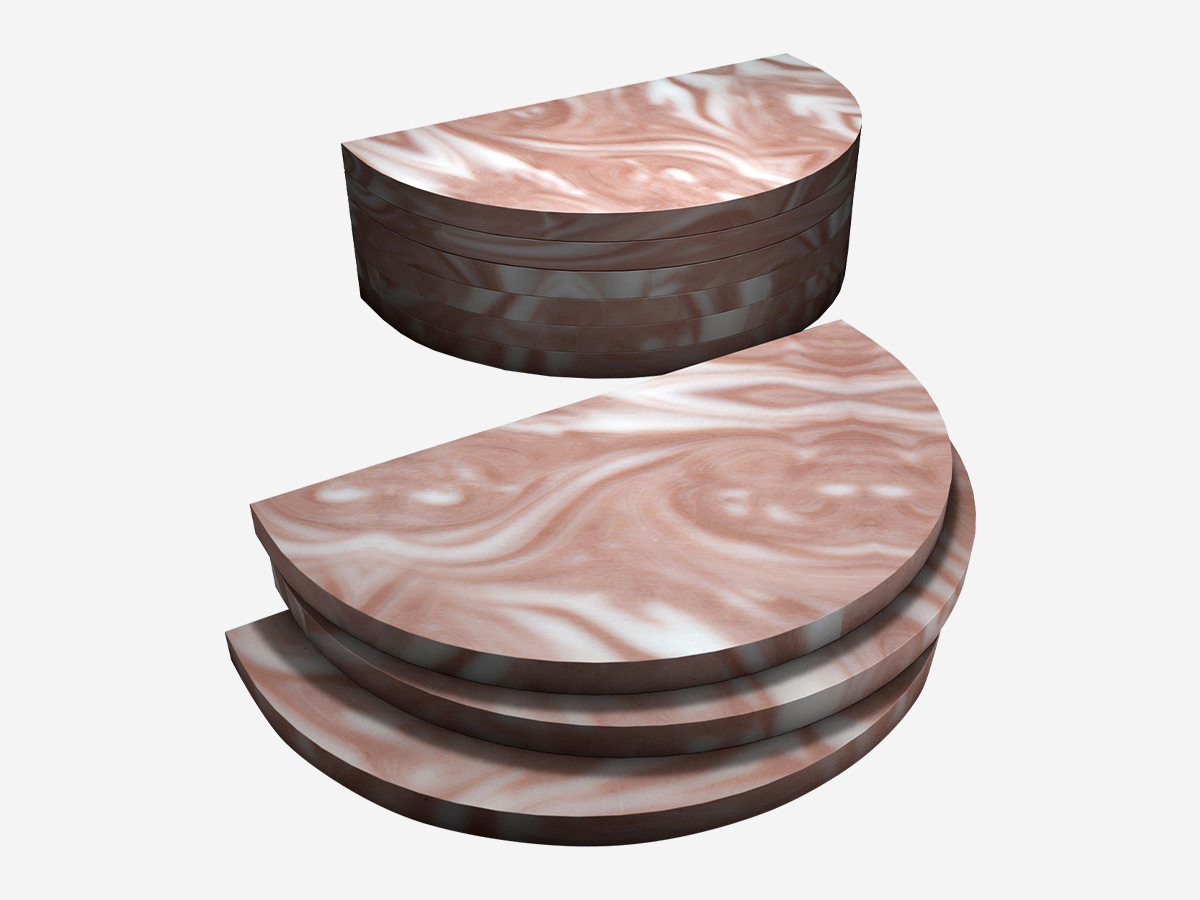
Mammography Phototimer Consistency Testing Slabs
- Precise assessment of AEC system performance in accordance with ACR and MQSA recommendations
- Simulate real breast tissue over the range of energies used in mammography.

Single Exposure High Contrast Resolution Phantom
- Perpendicular bar pattern design for assessment of system resolution using a single exposure
- Reproducible positioning
- Breast equivalent phantom body materials

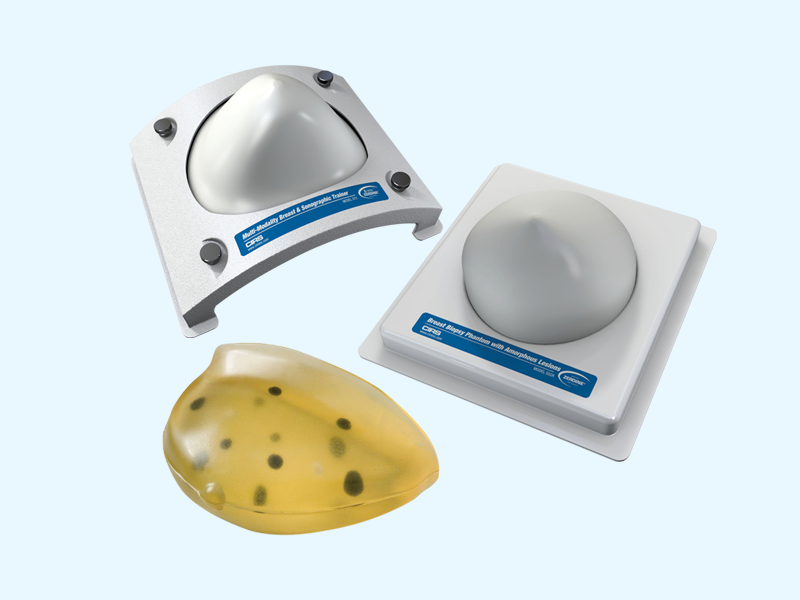
Tissue-equivalent Phantom for Mammography
- Test performance of any mammographic system
- Test objects range in size to allow system checks at varying levels of difficulty
- Monitor image quality & dose
BR3D Breast Imaging Phantom
- Tests Tomosynthesis and Breast Computed Tomography
- Complex background provides a greater challenge for target detection
- Slab configurations provide range of thicknesses with or without targets
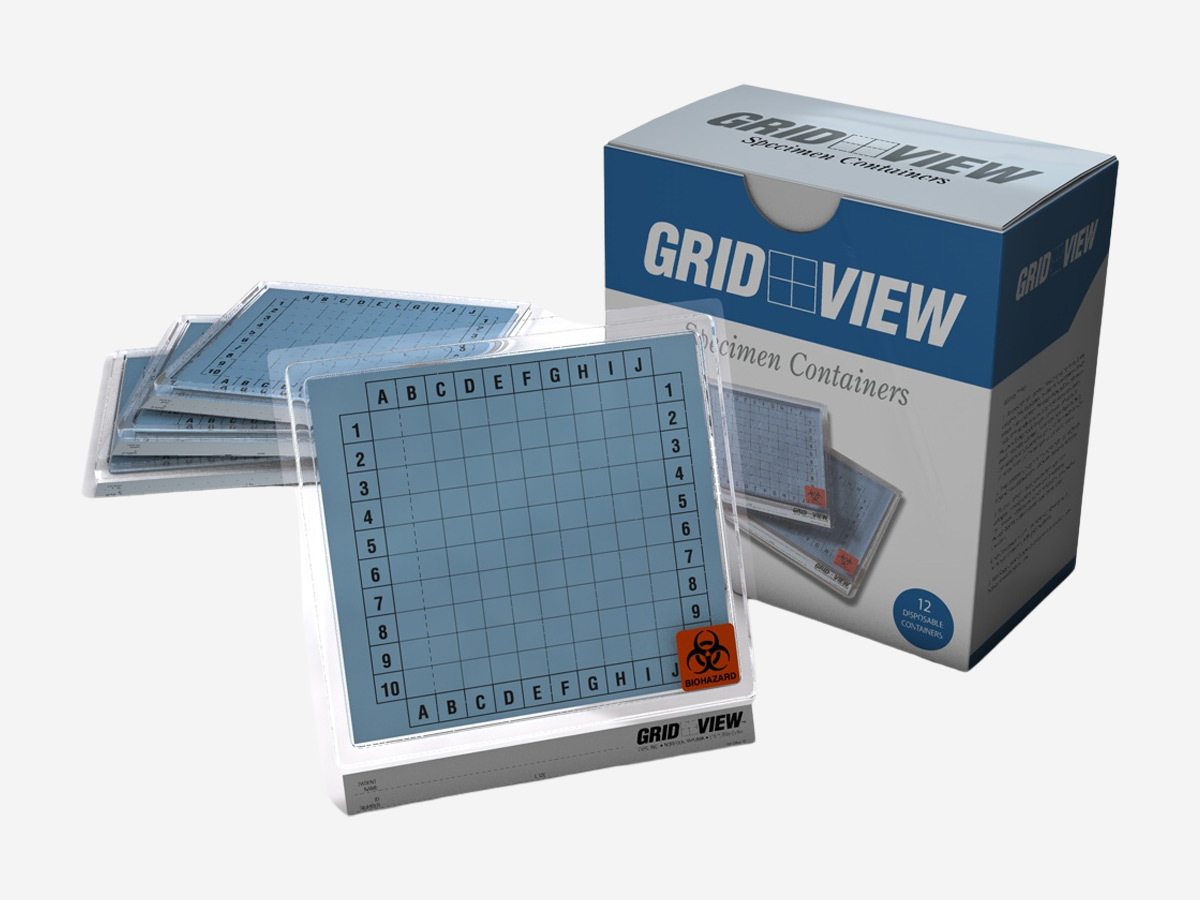
Grid View: Specimen Imaging and Transport Container
- Reduces surgery time through improved imaging turnaround
- Improves communication between surgery, radiology and pathology
- Eliminates the need for needles or wires
Ask us about these efficient Mammography QA tools.
Resources
Downloads
- Diagnostic Product Solutions Brochure
- Mammography Phototimer Consistency Testing Slabs Datasheet
- Single Exposure High Contrast Resolution Phantom Datasheet
- Tissue-Equivalent Phantom for Mammography Datasheet
- BR3D Breast Imaging Phantom Datasheet
- Grid View: Specimen Imaging and Transport Container Datasheet
- MoreLess
Specifications
Accuracy |
±0.01 lb [0 - 2 lb], ±0.02 lb [2 - 75 lb] ±0.005 kg [0 - 1 kg], ±0.01 kg [1 - 34 kg] |
Display Units |
g, lb:oz, kg, lb, oz |
Scale Dimensions |
8.9 x 8.2 x 2.9 in (225 x 208 x 73 mm) |
Foam Compression Block (included) |
Polyethylene Foam |
Scale Weight |
2 lbs. (0.95 kg) |
Power |
Alkaline Batteries Size C (4x), not included |
RoHS Compliant, CE Mark |
Yes |
Case |
Optional Soft Case 163-DIG-SC, not included |
| MoreLess | |
Construction |
99.99% Pure Aluminum |
Size |
10 x 10 cm (4 x 4 in) |
Weight |
0.09 kg (0.2 lbs) |
Thickness |
0.1 mm |
Construction |
High Purity Aluminum Alloy and Copper, 9 steps 0.3 mm high x 1.4 cm deep |
Size |
14.2 x 4 cm (5.6 x 1.9 in) |
Weight |
10 g (0.4 oz) |
Construction |
7 pieces of Acrylic (Phototimer Consistency Tools) |
Phototimer Consistency Tools Sizes |
3 each of 14 x 14 x 1.90 cm ± 2.0 mm; |
Phototimer Consistency Tools-BR Sizes |
3 each of 14 x 14 x 2 cm ± 0.2 mm; |
Weight |
Phototimer Consistency Tools: 2.3 kg (4.3 lbs) |
Screen Size |
24 x 30 cm (9.4 x 11.8 in) |
Mesh |
#40 Mesh - Copper |
Size |
25.8 x 31.5 cm (10.2 x 12.4 in) |
Weight |
0.4 kg (0.9 lbs) |
Set Dimensions |
12.5 cm x 10 cm x 4.5 cm |
Weight |
2 lbs. (0.7 kg) |
Materials |
Phantom: BR12 |
Dimensions |
18.5 L x 12.5 H x 4.5cm W |
Weight |
2 lbs. (0.7 kg) |
Materials |
Phantom: Epoxy Resin |
Overall Dimensions |
100 mm x 180 mm x 60 mm |
Individual Slab Dimensions |
100 mm x 180 mm x 10 mm, semicircular shape |
Weight |
0.88 kg (1.94 lb) |
Materials |
Slabs: epoxy resin |
Dimensions |
16 cm x 10.8 cm x 10.8 cm |
Weight |
0.5 lbs. (0.18 kg) |
Materials |
Transparent Plastic |